Preventing Facial Pressure Injuries in Prone Position Patient

Specialized surface reduces pressure injuries, optimizes ICU workflow, lessens workload, and enhances outcomes during prone ventilation.
Treating ARDS with prone position ventilation
Prone position has been frequently used in the intensive care units to improve the prognosis in patients with acute respiratory distress syndrome (ARDS). Regarding the American journal of respiratory and critical care medicine (AJRCCM) practice guideline, patients treated in a prone position during mechanical ventilation are usually in a prone position for prolonged periods >12 hours per day.1
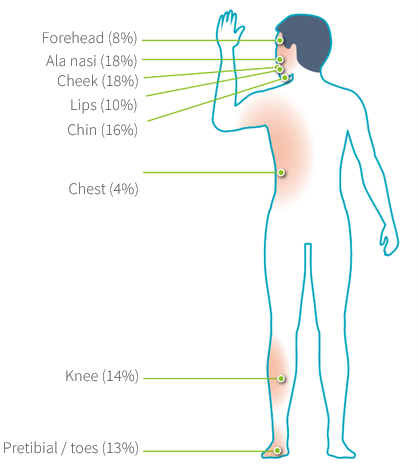
The face is the most severely affected area in prone position
Prone positioning during mechanical ventilation is consequently strongly recommended in adults with ARDS, however, turning patients to prone imply important complications such as pressure injuries. The incidence of pressure injuries is higher in prone position versus in the supine position. Prone positioning significantly increases pressure injury risk in vulnerable areas. The face was the most affected region (70%).2 Thus, ensuring the patient is correctly positioned and protected from injury is a crucial activity.
- Use a pressure redistribution support surface or positioning devices to offload pressure points on the face and body while in the prone position. Once positioned check for uneven distribution of pressure and positioning of medical devices if possible. Pay particular attention to breast region, knees, toes, penis, clavicles, iliac crest and symphysis pubis.
- Consider using additional pressure injury prevention strategies such as prophylactic dressing under devices and over bony prominences (e.g., the iliac crest, ribs and patella).
- At each rotation, assess the face and other body areas (i.e., breast region, knees, toes, penis, clavicles, iliac crest and symphysis pubis) that may be at risk when individuals are in the prone position.
Since pressure injury risk associated with patient’s head is significantly higher in prone position, the National Pressure Injury Advisory Panel (NPIAP) suggests that use of appropriate support surfaces and pillows and repositioning as soon as feasible is important when the prone position cannot be avoided. Optima Prone mattress provides headrest with an ergonomic facial pillow, a sculpted pocket, and alternating pressure shelters ear and cushions face are specifically designed (Patent no. EP4049641B1 ) for ear protection and throat protection to prevent pressure sore or injury risk on the vulnerable area.

"Optima Prone" Solution for Pressure Injuries in Prone Position.
It provides the following benefits for pressure injury prevention:
1. Protect patient’s face & ear:
Headrest with an ergonomic facial pillow, a sculpted pocket, and alternating pressure shelters ear and cushions face, reducing the reducing the risk of pressure injury complications.
2. Protect patient's vulnerable areas:
Control over individual air cell airflow allows zero pressure and personalized care to vulnerable areas, preventing pressure-induced injuries and avoiding excess pressure in the abdomen area to improve respiratory system function.
3. Uphold patient care quality:
Exclusive cell deflation card and timer feature allow convenient pressure setting tracking, helping caregivers maintain therapy consistency and accuracy.
If want to know about Optima Prone
Optima Prone - Support Surfaces - Pressure Area Care | Wellell Explore the Impact of Pressure Injuries on your hospital
https://www.wellell.com/en/how-can-we-help
References:
1. Fan, Eddy et al. “An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: Mechanical Ventilation in Adult Patients with Acute Respiratory Distress Syndrome.” American journal of respiratory and critical care medicine vol. 195,9 (2017): 1253-1263. doi:10.1164/rccm.201703-0548ST
2. Ibarra G, Rivera A, Fernandez-Ibarburu B, Lorca-García C, Garcia-Ruano A. Prone position pressure sores in the COVID-19 pandemic: The Madrid experience. Journal of Plastic, Reconstructive & Aesthetic Surgery : JPRAS. 2021 Sep;74(9):2141-2148. DOI: 10.1016/j.bjps.2020.12.057. PMID: 33446462; PMCID: PMC7837206.
3. European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline. Emily Haesler (Ed.). EPUAP/NPIAP/PPPIA; 2019.

